Melasma: A Step-by-Step Approach to Multimodal Treatment
By Dr. Wolfgang G. Philipp-Dormston
Overview
Melasma is a complex and chronic skin condition that causes symmetric dark patches on sun-exposed areas of the face. Although it’s benign, melasma can have a considerable psychological and emotional impact due to its visibility and tendency to recur. This review presents a modern, step-by-step guide to diagnosing and treating melasma using a combination of therapies tailored to each patient’s needs.
Understanding Melasma
Melasma (also called chloasma) appears as brown or grayish patches, typically on the cheeks, forehead, upper lip, or jawline. While most common in women, especially during their 30s and 40s, men can also be affected. The condition is more prevalent in individuals with medium to dark skin tones (Fitzpatrick skin types III–V) and is strongly influenced by genetics, sun exposure, and hormones.
Key Aggravating Factors:
• Sunlight (UV and visible light)exposure
• Hormonal changes(e.g., pregnancy, contraceptive pills, hormone therapies)
• Genetic predisposition
• Photosensitizing medications and cosmetics
• Stress, inflammation, and certain diseases(like PCOS or thyroid dysfunction)
Diagnosis and Assessment
The diagnosis of melasma is mainly clinical, based on the appearance of the lesions and patient history. However, advanced diagnostic tools can improve precision:
• Wood’s lamp: Helps determine if pigmentation is epidermal (superficial) or dermal (deeper).
• Dermoscopy: Highlights pigment distribution.
• Reflectance Confocal Microscopy (RCM)or Dynamic Optical Coherence Tomography (D-OCT): Non-invasive tools that allow visualization of skin structures, including melanocyte activity and blood vessel changes.
To guide treatment, it is also important to rule out other similar conditions such as post-inflammatory hyperpigmentation, lichen planus pigmentosus, and drug-induced pigmentation.
Step-by-Step Treatment Approach
Due to melasma’s complex pathophysiology, treatment must be multimodal—targeting pigment production, inflammation, vascular factors, and hormonal influences.
Step 1: Strict Photoprotection
Sunlight, especially UVA and high-energy visible light (HEVL), is a major trigger. Daily use of broad-spectrum sunscreens with SPF 30+ is essential. Products containing iron oxide offer additional HEVL protection and are particularly beneficial. Avoidance of tanning beds and protective clothing is also recommended.
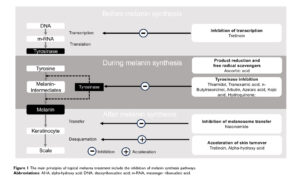
Step 2: Topical Treatments (First-line Therapy)
Tyrosinase Inhibitors
These block the enzyme responsible for melanin production. Preferred agents include:
• Thiamidol– considered one of the most effective human tyrosinase inhibitors.
• Tranexamic Acid (TXA)– has anti-inflammatory and anti-vascular benefits.
• Azelaic acid, arbutin, cysteamine, kojic acid– effective but may have higher irritation potential or regulatory concerns.
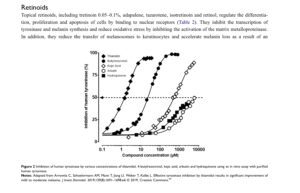
Retinoids (e.g., tretinoin, adapalene, retinol)
Retinoids help by increasing skin turnover, reducing melanin transfer, and enhancing penetration of other active ingredients. Results typically appear after 12–24 weeks. Mild irritation is common.
Niacinamide (Vitamin B3)
Reduces pigment transfer and inflammation, supports the skin barrier, and improves overall skin texture.
Antioxidants
Topical or oral vitamin C, pycnogenol, ferulic acid, and other plant-derived antioxidants help neutralize oxidative stress, a key contributor to pigmentation.
Step 3: Chemical Peels (Second-line Therapy)
Peels, including glycolic acid, salicylic acid, lactic acid, and trichloroacetic acid (TCA), exfoliate the skin and accelerate melanin removal. When used carefully, they can enhance the effect of topical treatments. However, they should be used cautiously in patients with darker skin to avoid post-inflammatory hyperpigmentation.
Step 4: Procedural Therapies
Used when topical treatments alone are insufficient:
Microneedling and RF (Radiofrequency)
Microneedling creates microchannels that boost the absorption of actives like TXA. When combined with RF, it promotes collagen production, reduces vascularity, and improves skin texture. It’s especially effective when paired with topical TXA.
Lasers and Light-Based Devices
• Non-ablative fractional lasers (NAFLs)and picosecond lasersbreak down pigment without damaging the skin.
• Intense Pulsed Light (IPL)and Q-switched lasersoffer faster results but have higher recurrence and side effect risks, especially in darker skin types.
• Combining lasers with tyrosinase inhibitorsmay enhance long-term efficacy.
Step 5: Oral Treatments (Supportive Role)
Oral Tranexamic Acid (TXA)
Used in low doses, TXA can reduce melanin formation and vascular changes. However, side effects (e.g., menstrual irregularities, headaches, GI issues, and possible clotting risks) limit its use. It is often reserved for stubborn cases under medical supervision.
Maintenance and Patient Counseling
Even with good results, melasma is likely to recur if treatment stops or triggers return. Ongoing maintenance with photoprotection, mild topical agents, and regular follow-ups is crucial. Educating patients about the chronic nature of the condition, setting realistic expectations, and discussing possible side effects will improve treatment satisfaction and adherence.
Conclusion
Melasma management requires patience, expertise, and a tailored multimodal plan. A successful approach should combine:
• Consistent photoprotection
• Evidence-based topical therapies(especially newer and safer agents like thiamidol or TXA)
• Adjunctive treatments such as chemical peels, microneedling, and lasers
• Cautious use of oral agentswhen necessary
Because no single treatment is universally effective, an individualized plan that considers skin type, melasma severity, and lifestyle factors will yield the best outcomes.
Tamega Ade A, Miot LD, Bonfietti C, Gige TC, Marques ME, Miot HA. Clinical patterns and epidemiological characteristics of facial melasma in
Brazilian women. J Eur Acad Dermatol Venereol. 2013;27(2):151–156. doi:10.1111/j.1468-3083.2011.04430.x
2. Mandry Pagan R, Sanchez JL. Mandibular melasma. PR Health Sci J. 2000;19(3):231–234.
3. Ogbechie-Godec OA, Elbuluk N. Melasma: an up-to-date comprehensive review. Dermatol Ther. 2017;7(3):305–318. doi:10.1007/s13555-017-0194-1
4. Pawaskar MD, Parikh P, Markowski T, McMichael AJ, Feldman SR, Balkrishnan R. Melasma and its impact on health-related quality of life in
Hispanic women. J DermatolTreat. 2007;18(1):5–9. doi:10.1080/09546630601028778
5. Platsidaki E, Efstathiou V, Markantoni V, et al. Self-esteem, depression, anxiety and quality of life in patients with melasma living in a sunny
Mediterranean area: results from a prospective cross-sectional study. Dermatol Ther. 2023;13(5):1127–1136. doi:10.1007/s13555-023-00915-1
6. Piętowska Z, Nowicka D, Szepietowski JC. Understanding melasma – how can pharmacology and cosmetology procedures and prevention help
to achieve optimal treatment results? A narrative review. Int J Environ Res Public Health. 2022;19(19):12084. doi:10.3390/ijerph191912084
7. Bagherani N, Gianfaldoni S, Smoller BR. An overview on melasma. J Pigment Disord. 2015;2(10):218.
8. Sarkar R, Ailawadi P, Garg S. Melasma in men: a review of clinical, etiological, and management issues. J Clin Aesthetic Dermatol.
2018;11:53–59.
9. Deshpande SS, Khatu SS, Pardeshi GS, Gokhale NR. Cross-sectional study of psychiatric morbidity in patients with melasma. Indian
J Psychiatry. 2018;60(3):324–328. doi:10.4103/psychiatry.IndianJPsychiatry_115_16
10. Kang HY, Suzuki I, Lee DJ, et al. Transcriptional profiling shows altered expression of Wnt Pathway– and lipid Metabolism–Related genes as
well as melanogenesis-related genes in melasma. J Investig Dermatol. 2011;131(8):1692–1700. doi:10.1038/jid.2011.109
11. Mishra SN, Dhurat RS, Deshpande DJ, Nayak CS. Diagnostic utility of dermatoscopy in hydroquinone-induced exogenous ochronosis.
Int J Dermatol. 2013;52(4):413–417. doi:10.1111/j.1365-4632.2011.05305.x
12. Grimes PE, Yamada N, Bhawan J. Light microscopic, immunohistochemical, and ultrastructural alterations in patients with melasma. Am
J Dermatopathol. 2005;27(2):96–101. PubMed PMID: 15798432. doi:10.1097/01.dad.0000154419.18653.2e
13. Kang HY, Bahadoran P, Suzuki I, et al. In vivo reflectance confocal microscopy detects pigmentary changes in melasma at a cellular level
resolution. Exp Dermatol. 2010;19(8):e228–e233. doi:10.1111/j.1600-0625.2009.01057.x
14. Farabi B, Khan S, Jamgochian M, Atak MF, Jain M, Rao BK. The role of reflectance confocal microscopy in the diagnosis and management of
pigmentary disorders: a review. J Cosmet Dermatol. 2023;22(12):3213–3222. doi:10.1111/jocd.15827
15. Pomerantz H, Christman MP, Bloom BS, et al. Dynamic optical coherence tomography of cutaneous blood vessels in melasma and vessel
response to oral tranexamic acid. Lasers Surg Med. 2021;53(6):861–864. doi:10.1002/lsm.23345
16. Rodrigues M, Pandya AG. Melasma: clinical diagnosis and management options. Australas J Dermatol. 2015;56(3):151–163. doi:10.1111/
ajd.12290
17. Neagu N, Conforti C, Agozzino M, et al. Melasma treatment: a systematic review. J DermatolTreat. 2022;33(4):1816–1837. doi:10.1080/
09546634.2021.1914313
18. Searle T, Al-Niaimi F, Ali FR. The top 10 cosmeceuticals for facial hyperpigmentation. Dermatol Ther. 2020;33(6):e14095. doi:10.1111/
dth.14095
19. Effron C, Briden ME, Green BA. Enhancing cosmetic outcomes by combining superficial glycolic acid (alpha-hydroxy acid) peels with
nonablative lasers, intense pulsed light, and trichloroacetic acid peels. Cutis. 2007;79:4–8.
20. Griffiths C, Finkel LJ, Ditre CM, Hamilton TA, Ellis C, Voorhees J. Topical tretinoin (retinoic acid) improves melasma. A vehicle-controlled,
clinical trial. Br J Dermatol. 1993;129(4):415–421. doi:10.1111/j.1365-2133.1993.tb03169.x
21. Kimbrough-Green CK, Griffiths CE, Finkel LJ, et al. Topical retinoic acid (tretinoin) for melasma in black patients. A vehicle-controlled clinical
trial. Arch Dermatol. 1994;130(6):727–733. doi:10.1001/archderm.1994.01690060057005
22. Green C, Orchard G, Cerio R, et al. A clinicopathological study of the effects of topical retinyl propionate cream in skin photoageing. Clin Exp
Dermatol. 1998;23(4):162–167. doi:10.1046/j.1365-2230.1998.00331.x
23. Leenutaphong V, Nettakul A, Rattanasuwon P. Topical isotretinoin for melasma in Thai patients: a vehicle-controlled clinical trial. J Med Assoc
Thai. 1999;82(9):868–875.
24. Yoshimura K, Momosawa A, Aiba E, et al. Clinical trial of bleaching treatment with 10% all-trans retinol gel. Dermatol Surg. 2003;29
(2):155–160. doi:10.1046/j.1524-4725.2003.29039.x
25. Khunger N, Sarkar R, Jain RK. Tretinoin peels versus glycolic acid peels in the treatment of Melasma in dark-skinned patients. Dermatol Surg.
2004;30(5):756–760. doi:10.1111/j.1524-4725.2004.30212.x
26. Watson REB, Long SP, Bowden JJ, Bastrilles JY, Barton SP, Griffiths CE. Repair of photoaged dermal matrix by topical application of
a cosmetic “antiageing” product. Br J Dermatol. 2008;158(3):472–477. doi:10.1111/j.1365-2133.2007.08364.x
27. Ghersetich I, Troiano M, Brazzini B, Arunachalam M, Lotti T. Melasma: treatment with 10% tretinoin peeling mask. J Cosmet Dermatol.
2010;9(2):117–121. doi:10.1111/j.1473-2165.2010.00488.x
28. Kang HY, Valerio L, Bahadoran P, Ortonne JP. The role of topical retinoids in the treatment of pigmentary disorders: an evidence-based review.
Am J Clin Dermatol. 2009;10(4):251–260. doi:10.2165/00128071-200910040-00005
29. Sorg O, Kasraee B, Salomon D, Saurat JH. The potential depigmenting activity of retinaldehyde. Dermatology. 2013;227(3):231–237.
doi:10.1159/000354294
30. Truchuelo MT, Jiménez N, Jaén P. Assessment of the efficacy and tolerance of a new combination of retinoids and depigmenting agents in the
treatment of melasma. J Cosmet Dermatol. 2014;13(4):261–268. doi:10.1111/jocd.12110
31. Rendon MI, Barkovic S. Clinical evaluation of a 4% hydroquinone + 1% retinol treatment regimen for improving melasma and photodamage in
Fitzpatrick skin types III-VI. J Drugs Dermatol. 2016;15(11):1435–1441.
32. Okubo T, Oyohikawa M, Futaki K, Matsukami M, Fujii A. The inhibitory effects of 4-N-butyl-resorcinol on melanogenesis. J Dermatol Sci.
1995;10(1):88. doi:10.1016/0923-1811(95)93865-X
33. Kim DS, Kim SY, Park SH, et al. Inhibitory effects of 4-n-butylresorcinol on tyrosinase activity and melanin synthesis. Biol Pharm Bull.
2005;28(12):2216–2219. doi:10.1248/bpb.28.2216
34. Khemis A, Kaiafa A, Queille-Roussel C, Duteil L, Ortonne JP. Evaluation of efficacy and safety of rucinol serum in patients with melasma:
a randomized controlled trial. Br J Dermatol. 2007;156(5):997–1004. doi:10.1111/j.1365-2133.2007.07814.x
35. Huh SY, Shin JW, Na JI, Huh CH, Youn SW, Park KC. Efficacy and safety of liposome-encapsulated 4-n-butylresorcinol 0.1% cream for the
treatment of melasma: a randomized controlled split-face trial. J Dermatol. 2010;37(4):311–315. doi:10.1111/j.1346-8138.2010.00787.x
36. Kolbe L, Mann T, Gerwat W, et al. 4-n-butylresorcinol, a highly effective tyrosinase inhibitor for the topical treatment of hyperpigmentation.
37. Madan Mohan NT, Gowda A, Jaiswal AK, et al. Assessment of efficacy, safety, and tolerability of 4-n-butylresorcinol 0.3% cream: an Indian
multicentric study on melasma. Clin Cosmet Invest Dermatol. 2016;9:21–27. doi:10.2147/CCID.S89451
38. Kwon SH, Yang JH, Shin JW, Park KC, Huh CH, Na JI. Efficacy of liposome-encapsulated 4-n-butylresorcinol and resveratrol cream in the
treatment of melasma. J Cosmet Dermatol. 2020;19(4):891–895. doi:10.1111/jocd.13080
39. Kim J, Kim J, Lee YI, Almurayshid A, Jung JY, Lee JH. Effect of a topical antioxidant serum containing vitamin C, vitamin E, and FA after
Q-switched 1064-nm Nd: YAG laser for treatment of environment-induced skin pigmentation. J Cosmet Dermatol. 2020;19(10):2576–2582.
doi:10.1111/jocd.13323
40. Polnikorn N. Treatment of refractory melasma with the MedLite C6 Q-switched Nd: YAG laser and alpha arbutin: a prospective study. J Cosmet
Laser Ther. 2010;12(3):126–131. doi:10.3109/14764172.2010.487910
41. Morag M, Nawrot J, Siatkowski I, et al. A double-blind, placebo-controlled randomized trial of Serratulae quinquefoliae folium, a new source
of β-arbutin, in selected skin hyperpigmentations. J Cosmet Dermatol. 2015;14(3):185–190. doi:10.1111/jocd.12147
42. Crocco EI, Veasey JV, Boin MF, Lellis RF, Alves RO. A novel cream formulation containing nicotinamide 4%, arbutin 3%, bisabolol 1%, and
retinaldehyde 0.05% for treatment of epidermal melasma. Cutis. 2015;96(5):337–342.
43. Baliña LM, Graupe K. The treatment of melasma. 20% azelaic acid versus 4% hydroquinone cream. Int J Dermatol. 1991;30(12):893–895.
doi:10.1111/j.1365-4362.1991.tb04362.x
44. Farshi S. Comparative study of therapeutic effects of 20% azelaic acid and hydroquinone 4% cream in the treatment of melasma. J Cosmet
Dermatol. 2011;10(4):282–287. doi:10.1111/j.1473-2165.2011.00580.x
45. Mazurek K, Pierzchała E. Comparison of efficacy of products containing azelaic acid in melasma treatment. J Cosmet Dermatol. 2016;15
(3):269–282. doi:10.1111/jocd.12217
46. Verallo-Rowell VM, Verallo V, Graupe K, Lopez-Villafuerte L, Garcia-Lopez M. Double-blind comparison of azelaic acid and hydroquinone in
the treatment of melasma. Acta Derm Venereol Suppl. 1989;143:58–61.
47. Mansouri P, Farshi S, Hashemi Z, Kasraee B. Evaluation of the efficacy of cysteamine 5% cream in the treatment of epidermal melasma:
a randomized double-blind placebo-controlled trial. Br J Dermatol. 2015;173(1):209–217. doi:10.1111/bjd.13424
48. Lee HK, Ha JW, Hwang YJ, Boo YC. Identification of L-cysteinamide as a potent inhibitor of tyrosinase-mediated dopachrome formation and
eumelanin synthesis. Antioxidants. 2021;10(8):1202. doi:10.3390/antiox10081202
49. Santos-Neto AG D, da Silva ÍCV, Melo CR, Santana AAM, de Albuquerque-Junior RLC. Is cysteamine use effective in the treatment of
melasma? A systematic review and meta-analysis. Dermatol Ther. 2022;35(12):e15961. doi:10.1111/dth.15961
50. Erbil H, Sezer E, Taştan B, Arca E, Kurumlu Z. Efficacy and safety of serial glycolic acid peels and a topical regimen in the treatment of
recalcitrant melasma. J Dermatol. 2007;34(1):25–30. doi:10.1111/j.1346-8138.2007.00211.x
51. Sarkar R, Garg V, Bansal S, Sethi S, Gupta C. Comparative evaluation of efficacy and tolerability of glycolic acid, salicylic mandelic acid, and
phytic acid combination peels in melasma. Dermatol Surg. 2016;42(3):384–391. doi:10.1097/DSS.0000000000000642
52. Sahu P, Dayal S. Most worthwhile superficial chemical peel for melasma of skin of color: authors’ experience of glycolic, trichloroacetic acid,
and lactic peel. Dermatol Ther. 2021;34(1):e14693. doi:10.1111/dth.14693
53. Chaudhary S, Dayal S. Efficacy of combination of glycolic acid peeling with topical regimen in treatment of melasma. J Drugs Dermatol.
2013;12(10):1149–1153.
54. Lim JTE. Treatment of melasma using kojic acid in a gel containing hydroquinone and glycolic acid. Dermatol Surg. 1999;25(4):282–284.
doi:10.1046/j.1524-4725.1999.08236.x
55. Hurley ME, Guevara IL, Gonzales RM, Pandya AG. Efficacy of glycolic acid peels in the treatment of melasma. Arch Dermatol. 2002;138
(12):1578–1582. doi:10.1001/archderm.138.12.1578
56. Ilknur T, Biçak MU, Demirtaşoğlu M, Ozkan S. Glycolic acid peels versus amino fruit acid peels in the treatment of melasma. Dermatol Surg.
2010;36(4):490–495. doi:10.1111/j.1524-4725.2010.01481.x
57. Faghihi G, Shahingohar A, Siadat AH. Comparison between 1% tretinoin peeling versus 70% glycolic acid peeling in the treatment of female
patients with melasma. J Drugs Dermatol. 2011;10(12):1439–1442.
58. Dayal S, Sahu P, Dua R. Combination of glycolic acid peel and topical 20% azelaic acid cream in melasma patients: efficacy and improvement
in quality of life. J Cosmet Dermatol. 2017;16(1):35–42. doi:10.1111/jocd.12260
59. Tse TW. Hydroquinone for skin lightening: safety profile, duration of use and when should we stop? J DermatolTreat. 2010;21(5):272–275.
doi:10.3109/09546630903341945
60. Guevara IL, Pandya AG. Safety and efficacy of 4% hydroquinone combined with 10% glycolic acid, antioxidants, and sunscreen in the
treatment of melasma. Int J Dermatol. 2003;42(12):966–972. doi:10.1111/j.1365-4632.2003.02017.x
61. Westerhof W, Kooyers TJ. Hydroquinone and its analogues in dermatology-A potential health risk. J Cosmet Dermatol. 2005;4(2):55–59.
doi:10.1111/j.1473-2165.2005.40202.x
62. Garcia A, Fulton JE. The combination of GA and hydroquinone or kojic acid for the treatment of melasma and related conditions. Dermatol
Surg. 1996;22(5):443–447. doi:10.1111/j.1524-4725.1996.tb00345.x
63. Monteiro RC, Kishore BN, Bhat RM, Sukumar D, Martis J, Ganesh HK. A comparative study of the efficacy of 4% hydroquinone vs 0.75%
kojic acid cream in the treatment of facial melasma. Indian J Dermatol. 2013;58(2):157. doi:10.4103/0019-5154.108070
64. Deo KS, Dash KN, Sharma YK, Virmani NC, Oberai C. Kojic acid vis-A-vis its combinations with hydroquinone and betamethasone valerate in melasma:
a randomized, single blind, comparative study of efficacy and safety. Indian J Dermatol. 2013;58(4):281–285. doi:10.4103/0019-5154.113940
65. Saghaie L, Pourfarzam M, Fassihi A, Sartippour B. Synthesis and tyrosinase inhibitory properties of some novel derivatives of kojic acid. Res
Pharm Sci. 2013;8(4):233–242.
66. Saeedi M, Eslamifar M, Khezri K. Kojic acid applications in cosmetic and pharmaceutical preparations. Biomed Pharmacother.
2019;110:582–593. doi:10.1016/j.biopha.2018.12.006
67. Scientific Committee on Consumer Safety. European Commission. Opinion on kojic acid; [updated June 26–27, 2012; cited December 12, 2023].
Available from: https://ec.europa.eu/health/sites/health/files/scientific_committees/consumer_safety/docs/sccs_o_098.pdf. Accessed April 26, 2024.
68. Mann T, Gerwat W, Batzer J, et al. Inhibition of human tyrosinase requires molecular motifs distinctively different from mushroom tyrosinase.
J Invest Dermatol. 2018;138(7):1601–1608. doi:10.1016/j.jid.2018.01.019
69. Arrowitz C, Schoelermann AM, Mann T, Jiang LI, Weber T, Kolbe L. Effective tyrosinase inhibition by thiamidol results in significant
improvement of mild to moderate melasma. J Invest Dermatol. 2019;139(8):1691–1698.e6. doi:10.1016/j.jid.2019.02.013
70. Roggenkamp D, Sammain A, Fürstenau M, Kausch M, Passeron T, Kolbe L. Thiamidol® in moderate-to-severe melasma: 24-week,
randomized, double-blind, vehicle-controlled clinical study with subsequent regression phase. J Dermatol. 2021;48(12):1871–1876.
doi:10.1111/1346-8138.16080
71. Philipp-Dormston WG, Vila Echagüe A, Pérez Damonte SH, et al. Thiamidol containing treatment regimens in facial hyperpigmentation: an
international multi-centre approach consisting of a double-blind, controlled, split-face study and of an open-label, real-world study. Int J Cosmet
Sci. 2020;42(4):377–387. doi:10.1111/ics.12626
72. Ebrahim HM, Said Abdelshafy A, Khattab F, Gharib K. Tranexamic acid for melasma treatment: a split-face study. Dermatol Surg. 2020;46(11):
e102–e107. doi:10.1097/DSS.0000000000002449
73. Bala HR, Lee S, Wong C, Pandya A, Rodrigues M. Oral tranexamic acid for the treatment of melasma: a review. Dermatol Surg. 2018;44
(6):814–825. doi:10.1097/DSS.0000000000001518
74. Janney MS, Subramaniyan R, Dabas R, Lal S, Das NM, Godara SK. A randomized controlled study comparing the efficacy of topical 5%
tranexamic acid solution versus 3% hydroquinone cream in melasma. J Cutan Aesthet Surg. 2019;12(1):63–67. doi:10.4103/JCAS.JCAS_40_18
75. Kim H, Moon S, Cho S, Lee J. Efficacy and safety of tranexamic acid in melasma: a meta-analysis and systematic review. Acta Derm Venereol.
2017;97(7):776–781. doi:10.2340/00015555-2668
76. Tan AWM, Sen P, Chua SH, Goh BK. Oral tranexamic acid lightens refractory melasma. Australas J Dermatol. 2017;58(3):e105–e108.
doi:10.1111/ajd.12474
77. Lee HC, Thng TGS, Goh CL. Oral tranexamic acid (TA) in the treatment of melasma: a retrospective analysis. J Am Acad Dermatol.
2016;75:385–392.
78. Wu S, Shi H, Wu H, et al. Treatment of melasma with oral administration of tranexamic acid. Aesthetic Plast Surg. 2012;36(4):964–970.
doi:10.1007/s00266-012-9899-9
79. Sahu PJ, Singh AL, Kulkarni S, Madke B, Saoji V, Jawade S. Study of oral tranexamic acid, topical tranexamic acid, and modified Kligman’s
regimen in treatment of melasma. J Cosmet Dermatol. 2020;19(6):1456–1462. doi:10.1111/jocd.13430
80. Lueangarun S, Sirithanabadeekul P, Wongwicharn P, et al. Intradermal tranexamic acid injection for the treatment of melasma: a pilot study with
48-week follow-up. J Clin Aesthet Dermatol. 2020;13(8):36–39.
81. Banihashemi M, Zabolinejad N, Jaafari MR, Salehi M, Jabari A. Comparison of therapeutic effects of liposomal Tranexamic Acid and
conventional Hydroquinone on melasma. J Cosmet Dermatol. 2015;14(3):174–177.
82. Laothaworn V, Juntongjin P. Topical 3% tranexamic acid enhances the efficacy of 1064-nm Q-switched neodymium-doped yttrium aluminum
garnet laser in the treatment of melasma. J Cosmet Laser Ther. 2018;20(6):320–325. doi:10.1080/14764172.2018.1427869
83. Xu Y, Ma R, Juliandri J, et al. Efficacy of functional microarray of microneedles combined with topical tranexamic acid for melasma:
a randomized, self-controlled, split-face study. Medicine. 2017;96(19):e6897. doi:10.1097/MD.0000000000006897
84. Saki N, Darayesh M, Heiran A. Comparing the efficacy of topical hydroquinone 2% versus intradermal tranexamic acid microinjections in
treating melasma: a split-face controlled trial. J DermatolTreat. 2018;29(4):405–410. doi:10.1080/09546634.2017.1392476
85. Tehranchinia Z, Saghi B, Rahimi H. Evaluation of therapeutic efficacy and safety of tranexamic acid local infiltration in combination with
topical 4% hydroquinone cream compared to topical 4% hydroquinone cream alone in patients with melasma: a split-face study. Dermatol Res
Pract. 2018;2018:8350317. doi:10.1155/2018/8350317
86. Budamakuntla L, Loganathan E, Suresh DH, et al. A randomised, open-label, comparative study of tranexamic acid microinjections and
tranexamic acid with microneedling in patients with melasma. J Cutan Aesthet Surg. 2013;6(3):139–143. doi:10.4103/0974-2077.118403
87. Sharma R, Mahajan VK, Mehta KS, Chauhan PS, Rawat R, Shiny TN. Therapeutic efficacy and safety of oral tranexamic acid and that of
tranexamic acid local infiltration with microinjections in patients with melasma: a comparative study. Clin Exp Dermatol. 2017;42(7):728–734.
doi:10.1111/ced.13164
88. Taylor SC, Torok H, Jones T, et al. Efficacy and safety of a new triple-combination agent for the treatment of facial melasma. Cutis. 2003;72(1):67–72.
89. Torok H, Taylor S, Baumann L, et al. A large 12-month extension study of an 8-week trial to evaluate the safety and efficacy of triple
combination (TC) cream in melasma patients previously treated with TC cream or one of its dyads. J Drugs Dermatol. 2005;4(5):592–597.
90. Ferreira Cestari T, Hassun K, Sittart A, de Lourdes Viegas M. A comparison of triple combination cream and hydroquinone 4% cream for the
treatment of moderate to severe facial melasma. J Cosmet Dermatol. 2007;6(1):36–39. doi:10.1111/j.1473-2165.2007.00288.x
91. Chan R, Park KC, Lee MH, et al. A randomized controlled trial of the efficacy and safety of a fixed triple combination (fluocinolone acetonide
0.01%, hydroquinone 4%, tretinoin 0.05%) compared with hydroquinone 4% cream in Asian patients with moderate to severe melasma. Br
J Dermatol. 2008;159(3):697–703. doi:10.1111/j.1365-2133.2008.08717.x
92. Gong Z, Lai W, Zhao G, et al. Efficacy and safety of fluocinolone acetonide, hydroquinone, and tretinoin cream in Chinese patients with
melasma: a randomized, double-blind, placebo-controlled, multicenter, parallel-group study. Clin Drug Investig. 2015;35(6):385–395.
doi:10.1007/s40261-015-0292-8
93. Arellano I, Cestari T, Ocampo-Candiani J, et al. Preventing melasma recurrence: prescribing a maintenance regimen with an effective triple
combination cream based on long-standing clinical severity. J Eur Acad Dermatol Venereol. 2012;26(5):611–618. doi:10.1111/j.1468-
3083.2011.04135.x
94. Grimes PE, Bhawan J, Guevara IL, et al. Continuous therapy followed by a maintenance therapy regimen with a triple combination cream for
melasma. J Am Acad Dermatol. 2010;62(6):962–967. doi:10.1016/j.jaad.2009.06.067
95. Sarkar R, Bansal S, Garg VK. Chemical peels for melasma in dark-skinned patients. J Cutan Aesthet Surg. 2012;5(4):247–253. doi:10.4103/
0974-2077.104912
96. Simmler C, Pauli GF, Chen SN. Phytochemistry and biological properties of glabridin. Fitoterapia. 2013;90:160–184. doi:10.1016/j.
fitote.2013.07.003
97. Yokota T, Nishio H, Kubota Y, Mizoguchi M. The inhibitory effect of glabridin from licorice extracts on melanogenesis and inflammation.
Pigment Cell Res. 1998;11(6):355–361. doi:10.1111/j.1600-0749.1998.tb00494.x
98. Zubair S, Mujtaba G. Comparison of efficacy of topical 2% liquiritin, topical 4% liquiritin and topical 4% hydroquinone in the management of
melasma. J Pak Assoc Dermatol. 2009;19:158–163.
99. Amer M, Metwalli M. Topical liquiritin improves melasma. Int J Dermatol. 2000;39(4):299–301. doi:10.1046/j.1365-4362.2000.00943.x
100. Huh CH, Seo KI, Park JY, Lim JG, Eun HC, Park KC. A randomized, double-blind, placebo-controlled trial of vitamin C iontophoresis in
melasma. Dermatology. 2003;206(4):316–320. doi:10.1159/000069943
101. Espinal-Perez LE, Moncada B, Castanedo-Cazares JP. A double-blind randomized trial of 5% ascorbic acid vs. 4% hydroquinone in melasma.
Int J Dermatol. 2004;43(8):604–607. doi:10.1111/j.1365-4632.2004.02134.x
102. Hwang S-W, Oh D-J, Lee D, Kim J-W, Park S-W. Clinical efficacy of 25% l-Ascorbic Acid (C’ensil) in the treatment of melasma. J Cutan Med
Surg. 2009;13(2):74–81. doi:10.2310/7750.2008.07092
103. Handog EB, Galang DA, de Leon-Godinez MA, Chan GP. A randomized, double-blind, placebo-controlled trial of oral procyanidin with
vitamins A, C, E for melasma among Filipino women. Int J Dermatol. 2009;48(8):896–901. doi:10.1111/j.1365-4632.2009.04130.x
104. Costa A, Silva C, Arruda L, Zaniboni M, Cordero T, Moisés T. The association of emblica, licorice, and belides is an effective alternative to
hydroquinone for the clinical treatment of melasma: P3205. J Am Acad Dermatol. 2010;62(3):AB119.
105. Al-Niaimi F, Chiang NYZ. Topical vitamin C and the skin: mechanisms of action and clinical applications. J Clin Aesthet Dermatol. 2017;10(7):14–17.
106. Menon A, Eram H, Kamath PR, Goel S, Babu AMA. Split face comparative study of safety and efficacy of microneedling with Tranexamic acid
versus microneedling with vitamin C in the treatment of melasma. Indian Dermatol Online J. 2019;11(1):41–45. doi:10.4103/idoj.IDOJ_22_19
107. Ismail ESA, Patsatsi A, Abd El-Maged WM, Nada EEAE. Efficacy of microneedling with topical vitamin C in the treatment of melasma.
J Cosmet Dermatol. 2019;18(5):1342–1347. doi:10.1111/jocd.12878
108. Taylor MB, Yanaki JS, Draper DO, Shurtz JC, Coglianese M. Successful short-term and long-term treatment of melasma and postinflammatory
hyperpigmentation using vitamin C with a full-face iontophoresis mask and a mandelic/malic acid skin care regimen. J Drugs Dermatol. 2013;12
(1):45–50.
109. Sarkar R, Arora P, Garg KV. Cosmeceuticals for hyperpigmentation: what is available? J Cutan Aesthet Surg. 2013;6(1):4–11. doi:10.4103/
0974-2077.110089
110. Lima PB, Dias JAF, Esposito ACC, Miot LDB, Miot HA. French maritime pine bark extract (pycnogenol) in association with triple combination
cream for the treatment of facial melasma in women: a double-blind, randomized, placebo-controlled trial. J Eur Acad Dermatol Venereol.
2021;35(2):502–508. doi:10.1111/jdv.16896
111. Zduńska K, Dana A, Kolodziejczak A, Rotsztejn H. Antioxidant properties of FA and its possible application. Skin Pharmacol Phys. 2018;31
(6):332–336. doi:10.1159/000491755
112. Ichihashi M, Funasaka Y, Ohashi A, et al. The inhibitory effect of DL-alpha-tocopheryl ferulate in lecithin on melanogenesis. Anticancer Res.
1999;19(5A):3769–3774.
113. Funasaka Y, Komoto M, Ichihashi M. Depigmenting effect of alpha-tocopheryl ferulate on normal human melanocytes. Pigment Cell Res.
2003;13(Suppl. 8):170–174.
114. Tirado-Sánchez A, Santamaría-Román A, Ponce-Olivera RM. Efficacy of dioic acid compared with hydroquinone in the treatment of melasma.
Int J Dermatol. 2009;48(8):893–895. doi:10.1111/j.1365-4632.2009.04105.x
115. Navarrete-Solís J, Castanedo-Cázares JP, Torres-álvarez B, et al. A double-blind, randomized clinical trial of niacinamide 4% versus
hydroquinone 4% in the treatment of melasma. Dermatol Res Pract. 2011;2011:379173. doi:10.1155/2011/379173
116. Forbat E, Al-Niaimi F, Ali FR. Use of nicotinamide in dermatology. Clin Exp Dermatol. 2017;42(2):137–144. doi:10.1111/ced.13021
117. Wallo W, Nebus J, Leyden JJ. Efficacy of a soy moisturizer in photoaging: a double-blind, vehicle-controlled, 12-week study. J Drugs
Dermatol. 2007;6(9):917–922.
118. Hermanns JF, Petit L, Martalo O, Piérard-Franchimont C, Cauwenbergh G, Piérard GE. Unraveling the patterns of subclinical
pheomelanin-enriched facial hyperpigmentation: effect of depigmenting agents. Dermatology. 2000;201(2):118–122. doi:10.1159/000018473
119. Pierard G, Graf R, Gonzalez R, Cauwenbergh W. Effects of soy on hyperpigmentation in Caucasian and Hispanic populations. In: 59th Annual
Meeting of the American Academy of Dermatology; March 2–7; 2001; Washington, DC.
120. Soliman MM, Ramadan SA, Bassiouny DA, Abdelmalek M. Combined trichloroacetic acid peel and topical ascorbic acid versus trichloroacetic
acid peel alone in the treatment of melasma: a comparative study. J Cosmet Dermatol. 2007;6(2):89–94. doi:10.1111/j.1473-2165.2007.00302.x
121. Abdel-Majid EM, Helmy ER, Abdel Motaleb AA. Modified Jessner’s solution combined with trichloroacetic acid 20% versus glycolic acid 70%
combined with trichloroacetic acid 20% in the treatment of melasma. Dermatol Surg. 2021;47(5):e179–e183. doi:10.1097/DSS.0000000000002964
122. Abdel-Meguid AM, Taha EA, Ismail SA. Combined jessner solution and trichloroacetic acid versus trichloroacetic acid alone in the treatment of
melasma in dark-skinned patients. Dermatol Surg. 2017;43(5):651–656. doi:10.1097/DSS.0000000000001036
123. Murtaza F, Bangash AR, Khushdil A, Noor SM. Efficacy of trichloro-acetic acid peel alone versus combined topical magnesium ascorbyl
phosphate for epidermal melasma. J Coll Physicians Surg Pak. 2016;26(7):557–561.
124. Ando H, Ryu A, Hashimoto A, Oka M, Ichihashi M. Linoleic acid and alpha-linolenic acid lightens ultraviolet-induced hyperpigmentation of
the skin. Arch Dermatol Res. 1998;290(7):375–381. doi:10.1007/s004030050320
125. Kanwar AJ, Dhar S, Kaur S. Treatment of melasma with potent topical corticosteroids. Dermatology. 1994;188(2):170. doi:10.1159/000247129
126. Nassar AAE, Ibrahim AM, Mahmoud AA. Efficacy and safety of intralesional steroid injection in the treatment of melasma. J Cosmet
Dermatol. 2021;20(3):862–867. doi:10.1111/jocd.13628
127. Kirsch B, Hoesly PM, Jambusaria A, Heckman MG, Diehl NN, Sluzevich JC. Evaluating the efficacy, safety, and tolerability of the combination
of tazarotene, azelaic acid, tacrolimus, and zinc oxide for the treatment of melasma: a pilot study. J Clin Aesthet Dermatol. 2019;12(5):40–45.
128. Adalatkhah H, Sadeghi-Bazargani H. The first clinical experience on efficacy of topical flutamide on melasma compared with topical
hydroquinone: a randomized clinical trial. Drug Des Devel Ther. 2015;9:4219–4225. doi:10.2147/DDDT.S80713
129. Cohen PR. Melasma treatment: a novel approach using a topical agent that contains an anti-estrogen and a vascular endothelial growth factor
inhibitor. Med Hypotheses. 2017;101:1–5. doi:10.1016/j.mehy.2017.01.020
130. Dhaliwal S, Rybak I, Ellis SR, et al. Prospective, randomized, double-blind assessment of topical bakuchiol and retinol for facial photoageing.
Br J Dermatol. 2019;180(2):289–296. doi:10.1111/bjd.16918
131. Zasada M, Budzisz E. Retinoids: active molecules influencing skin structure formation in cosmetic and dermatological treatments. Postepy
Dermatol Alergol. 2019;36(4):392–397. doi:10.5114/ada.2019.87443
132. Ortonne JP. Retinoid therapy of pigmentary disorders. Dermatol Ther. 2006;19(5):280–288. doi:10.1111/j.1529-8019.2006.00085.x
133. Shroot B. Pharmacodynamics and pharmacokinetics of topical Adapalene. J Am Acad Dermatol. 1998;39(2):S17–S24. doi:10.1016/S0190-
9622(98)70440-2
134. Sharquie KE, Al-Mashhadani SA, Salman HA. Topical 10% zinc sulfate solution for treatment of melasma. Dermatol Surg. 2008;34
(10):1346–1349. doi:10.1111/j.1524-4725.2008.34287.x
135. Ni Z, Mu Y, Gulati O. Treatment of melasma with Pycnogenol®
. Phytother Res. 2002;16(6):567–571. doi:10.1002/ptr.1085
136. Babbush KM, Babbush RA, Khachemoune A. Treatment of melasma: a review of less commonly used antioxidants. Int J Dermatol. 2021;60
(2):166–173. doi:10.1111/ijd.15133
137. Balevi A, Ustuner P, Özdemir M. Salicylic acid peeling combined with vitamin C mesotherapy versus salicylic acid peeling alone in the
treatment of mixed type melasma: a comparative study. J Cosmet Laser Ther. 2017;19(5):294–299. doi:10.1080/14764172.2017.1314501
138. Conforti C, Zalaudek I, Vezzoni R, et al. Chemical peeling for acne and melasma: current knowledge and innovations. G Ital Dermatol
Venereol. 2020;155(3):280–285. doi:10.23736/S0392-0488.19.06425-3
139. Sarkar R, Arsiwala S, Dubey N, et al. Chemical peels in melasma: a review with consensus recommendations by Indian Pigmentary Expert
Group. Indian J Dermatol. 2017;62(6):578–584. doi:10.4103/ijd.IJD_490_17
140. Kroon MW, Wind BS, Beek JF, et al. Nonablative 1550-nm fractional laser therapy versus triple topical therapy for the treatment of melasma:
a randomized controlled pilot study. J Am Acad Dermatol. 2011;64(3):516–523. doi:10.1016/j.jaad.2010.01.048
141. Massaki ABMN, Eimpunth S, Fabi SG, Guiha I, Groff W, Fitzpatrick R. Treatment of melasma with the 1927-nm fractional thulium fiber laser:
a retrospective analysis of 20 cases with long-term follow-up. Lasers Surg Med. 2013;45(2):95–101. doi:10.1002/lsm.22100
142. Tourlaki A, Galimberti MG, Pellacani G, Bencini PL. Combination of fractional erbium-glass laser and topical therapy in melasma resistant to
triple-combination cream. J Dermatol Treat. 2014;25(3):218–222. doi:10.3109/09546634.2012.671911
143. Rho N-K. Treatment of melasma using a novel 1927 nm fractional thulium laser: a retrospective analysis of 68 Korean Patients. Med Lasers.
2017;6(1):10–16. doi:10.25289/ML.2017.6.1.10
144. Trivedi M, Yang F, Cho B. A review of laser and light therapy in melasma. Int J Women’s Dermatol. 2017;3(1):11–20. doi:10.1016/j.ijwd.2017.01.004
145. Ma W, Gao Q, Liu J, et al. Efficacy and safety of laser-related therapy for melasma: a systematic review and network meta-analysis. J Cosmet
Dermatol. 2023;22(11):2910–2924. doi:10.1111/jocd.16006
146. Choi Y-J, Nam J-H, Kim JY, et al. Efficacy and safety of a novel picosecond laser using combination of 1064 and 595 nm on patients with
melasma: a prospective, randomized, multicenter, split-face, 2% hydroquinone cream-controlled clinical trial. Lasers Surg Med. 2017;49
(10):899–907. doi:10.1002/lsm.22735
147. Chen Y-T, Lin E-T, Chang C-C, et al. Efficacy and safety evaluation of picosecond alexandrite laser with a diffractive lens array for treatment of melasma
in asian patients by VISIA imaging system. Photobiomodulation Photomed Laser Surg. 2019;37(9):559–566. doi:10.1089/photob.2019.4644
148. Manuskiatti W, Yan C, Tantrapornpong P, Cembrano KAG, Techapichetvanich T, Wanitphakdeedecha R. A prospective, split-face, randomized
study comparing a 755-nm picosecond laser with and without diffractive lens array in the treatment of melasma in asians. Lasers Surg Med.
2021;53(1):95–103. doi:10.1002/lsm.23312
149. Lin ET, Chiang HM, Lin BS, Huang YH, Chang CC. Photoaging reversibility in asian patients with melasma treated using picosecond lasers with
a diffractive lens array: a 1-year prospective observational cohort study. Dermatol Surg. 2021;47(1):e10–e14. doi:10.1097/DSS.0000000000002405
150. Park BJ, Jung YJ, Ro YS, Chang SE, Kim JE. Therapeutic effects of new pulsed-type microneedling radiofrequency for refractory facial
pigmentary disorders. Dermatol Surg. 2022;48(3):327–333. doi:10.1097/DSS.0000000000003367
151. Feng X, Su H, Xie J. The efficacy and safety of microneedling with topical tranexamic acid for melasma treatment: a systematic review and
meta-analysis. J Cosmet Dermatol. 2023;23(1):33–43.
152. Mamdouh Kamal Dawaud S, Hegab DS, Mohamed El Maghraby G, Ahmad El-Ashmawy A. Efficacy and safety of topical tranexamic acid
alone or in combination with either fractional carbon dioxide laser or microneedling for the treatment of melasma. Dermatol Pract Concept.
2023;13(3):e2023195. doi:10.5826/dpc.1303a195
153. Castanedo-Cazares JP, Hernandez-Blanco D, Carlos- Ortega B, Fuentes-Ahumada C, Torres-Alvarez B. Near-visible light and UV photoprotection
in the treatment of melasma: a double-blind randomized trial. Photodermatol Photoimmunol Photomed. 2014;30(1):35–42.
doi:10.1111/phpp.12086
154. Vazquez M, Sanchez JL. The efficacy of a broad-spectrum sunscreen in the treatment of melasma. Cutis. 1983;32(1):92.
155. Morgado-Carrasco D, Piquero-Casals J, Granger C, Trullàs C, Passeron T. Melasma: the need for tailored photoprotection to improve clinical
outcomes. Photodermatol Photoimmunol Photomed. 2022;38(6):515–521. doi:10.1111/phpp.12783
156. Pedroso AG, Furtado GRD, Barbosa KL. Niacinamide for the treatment of melasma: an integrative review of randomized clinical trials. Res Soc
Develop. 2022;11(11):e198111133581. doi:10.33448/rsd-v11i11.33581